Barriers to Care: Access, Stigma, and Cultural Perceptions
PRAY FIRST for all who hold public office to speak boldly and with compassion to address the mental health concerns of the nation.
Gracious words are like a honeycomb, sweetness to the soul and health to the body. Proverbs 16:24
Over the past few decades, mental health care in the United States has undergone a dramatic transformation. In the mid-20th century, treatment was largely institutional, with many individuals placed in long-term psychiatric hospitals—often under harsh conditions and with limited therapeutic support. The deinstitutionalization movement of the 1970s and 1980s aimed to shift care to community-based settings, but the infrastructure to support this transition was never fully developed. As a result, many individuals with mental illness were left without adequate care, contributing to homelessness and incarceration rates among this population.
Today, mental health care is more integrated into general health systems, with increased emphasis on outpatient services, telehealth, and peer-led support. Awareness has grown, and stigma has lessened, especially among younger generations. However, access remains uneven, particularly in rural areas and among marginalized communities. The rise of digital platforms has created both challenges and opportunities, while social media can exacerbate anxiety, it also offers new avenues for support and education. Federal initiatives like the 988 Suicide & Crisis Lifeline and Certified Community Behavioral Health Clinics (CCBHCs) have helped expand crisis care and enforce parity laws, but systemic gaps persist, especially in workforce shortages and Medicaid coverage.
Access to Care: The Fractured System and Stigmas
Awareness has grown, but treatment gaps tell a harsher reality. According to Mental Health America’s 2024 report, nearly one in five adults—around 60 million people—live with mental illness, yet more than half go untreated. The divide is deepest in rural areas, where long drives, broadband gaps, and provider shortages make even telehealth feel out of reach. Community hubs—schools, churches, small nonprofits—often carry much of the responsibility, but most have little capacity to take on more.
Research shows notable differences in how generations approach mental health. Surveys indicate younger adults are more likely to discuss their feelings openly, seek therapy, and view counseling as a proactive step toward well-being. At the same time, older adults, veterans, and frontline workers often report barriers such as stigma, cultural expectations, and limited access to resources. Social media also adds another layer where studies have linked excessive screen time and comparison-driven content to increased anxiety. However, these same platforms can also host supportive communities and mental health resources that many find helpful.
Progress has not erased shame. The CDC identifies stigma on three fronts: public, self, and structural with each still creating barriers to care. Fear of being labeled “broken,” of losing jobs, or of betraying cultural expectations can keep many from seeking care. Research indicated that fear of judgment remains a major reason many individuals, particularly in certain communities, avoid seeking mental health care.
Building Better Paths Forward
Solutions are taking shape. Peer-led support groups, faith-based networks, and mobile clinics are broadening access. Experts suggest small, practical first steps for those hesitant: open up to someone you trust, call a helpline, or try a free mental health app. Despite increased awareness, access to mental health care remains limited due to provider shortages and other systemic barriers.
Breaking myths is crucial. Asking for help is not a weakness. Coping looks different for everyone—walking trails, journaling, prayer, music, setting small goals, and more. These little successes can feel like survival strategies in an overwhelming world.
Federal Response
Over the past decade, the U.S. federal government has taken major steps in strengthening mental health care, signaling a growing commitment to holistic well-being. Landmark initiatives like the 988 Suicide & Crisis Lifeline, launched in 2022, have created a nationwide safety net for individuals facing mental health and substance use crises. The expansion of Certified Community Behavioral Health Clinics (CCBHCs) has brought integrated, 24/7 care to communities across the country, while tighter enforcement of mental health parity laws ensures that mental health is treated with the same urgency and respect as physical health. These efforts reflect a cultural shift, one that increasingly values mental wellness as essential to a thriving society.
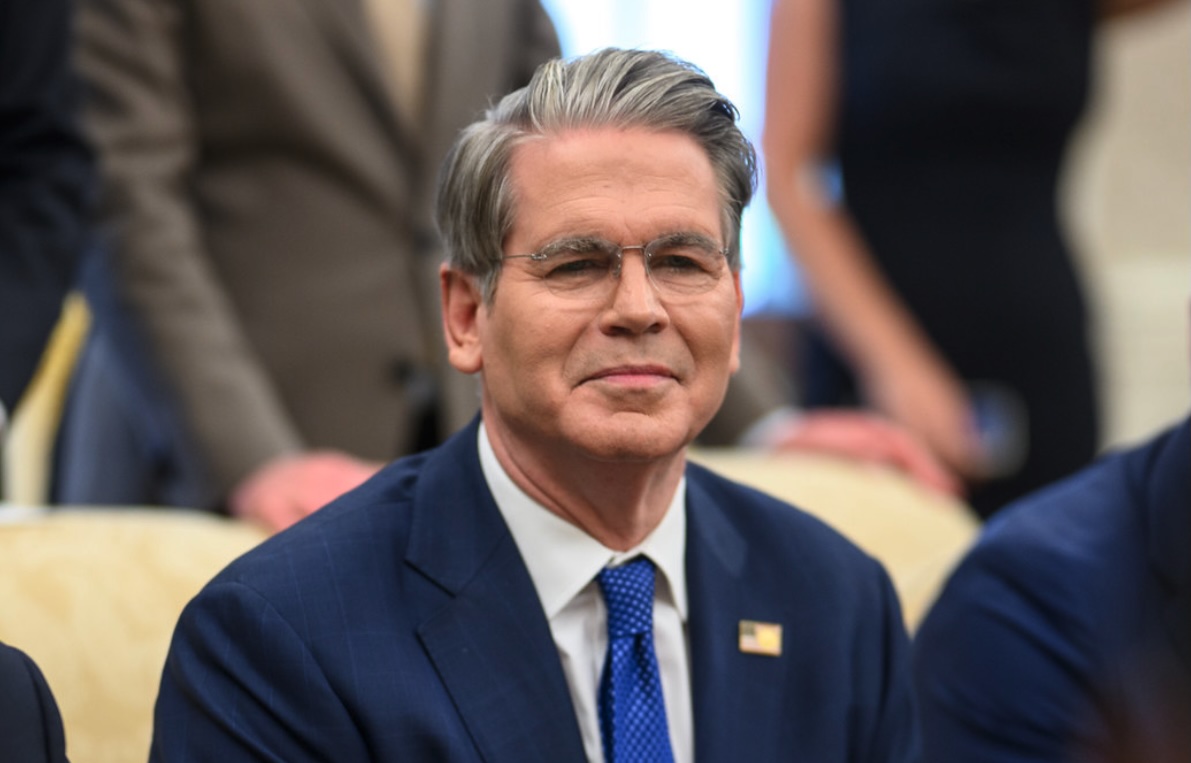
While challenges remain, especially for veterans and underserved populations, there is a growing momentum toward solutions. The Make America Healthy Again (MAHA) initiative, introduced by President Donald Trump and Health and Human Services Secretary Robert F. Kennedy Jr., has sparked a national conversation about the root causes of mental illness. By focusing on chronic disease prevention, nutrition, and environmental health, MAHA aims to build a foundation for long-term mental resilience. Though some policy changes, like the restructuring of the Substance Abuse and Mental Health Services Administration (SAMHSA) and shifts in funding, have raised concerns, the administration has also launched over 120 health initiatives that prioritize transparency, innovation, and community-based care.
Looking ahead, the future of mental health care in America is one of collaboration, creativity, and compassion. As public awareness grows and new models of care emerge, there is real potential to close treatment gaps, reduce stigma, and empower individuals to seek help without fear. With continued advocacy and thoughtful policy, the nation is poised to build a mental health system that truly supports every person who needs help.
Why It Matters and How We Can Respond
Mental health is not an abstract policy debate. It’s personal. People suffer quietly in the pew behind us, the neighbor across the street, the colleague on the other end of a Zoom call. Scripture calls us to more than awareness but to “Bear one another’s burdens, and so fulfill the law of Christ” (Galatians 6:2). That means listening without judgment, choosing words that heal rather than dismiss, and speaking truth with grace: “Let your speech always be gracious, seasoned with salt” (Colossians 4:6). Responding well also means practical action by advocating for mental health resources, supporting local care networks, and making room for honest conversations in our homes and churches—conversations that begin with “I see you” instead of silence.
HOW THEN SHOULD WE PRAY:
— Pray for agencies as they work to ensure that resources reach the underserved and under-resourced. Open your hand to the needy and satisfy the desire of the afflicted. Psalm 145:16
— Pray for those who are struggling with mental health issues, that they would find God’s hope in their silent battles. Though I walked in the midst of trouble, you preserve my life. Psalm 138:7
CONSIDER THESE ITEMS FOR PRAYER:
- Pray for all Americans to have discernment and grace to walk alongside others with understanding.
- Pray for federal leaders to seek God’s wisdom to speak truth in ways that heal rather than harm.
- Pray for healthcare providers to serve those in need with integrity and humility.
Sources: National Institute of Mental Health, Mental Health America, National Center for Biotechnology Information, National Library of Medicine, National Institutes of Health, Centers for Disease Control and Prevention, Time Magazine, Verywell Health